
5 Ways We Can Keep Your Immune System Strong
December 10, 2025/by Kaplan Center
Want to Take Your Workout to the Next Level Next Year? These Tips Can Help
December 8, 2025/by Kaplan Center
Dr. Kaplan’s Dos and Don’ts of the Holiday Season
December 3, 2025/by Kaplan Center
Let’s Talk Webinar – A Root Cause Q&A
December 2, 2025/by Kaplan Center
Navigating Holiday Meals with Gut Issues: Simple Tips for a Comfortable Season
December 1, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
Craniosacral Therapy for TMJ | Say Goodbye to the Daily Grind
November 19, 2025/by Patricia Alomar, M.S., P.T.
From Compassionate Care to Personal Healing: A Letter to My Patients
November 18, 2025/by Kaplan Center
8 Steps to a Healthier Gut—and a Longer, Healthier Life
November 18, 2025/by Kaplan Center
Mid-Life Irritability & Fatigue Improved by Hormonal Balancing
November 13, 2025/by Lisa Lilienfield, MD
From Challenges to Change: Dr. Kaplan on Healthcare’s Biggest Challenges
October 29, 2025/by Kaplan Center
Overlooked Dangers of Mold Exposure and How to Stay Safe – Dr. Kaplan Talks to WUSA9
October 27, 2025/by Kaplan Center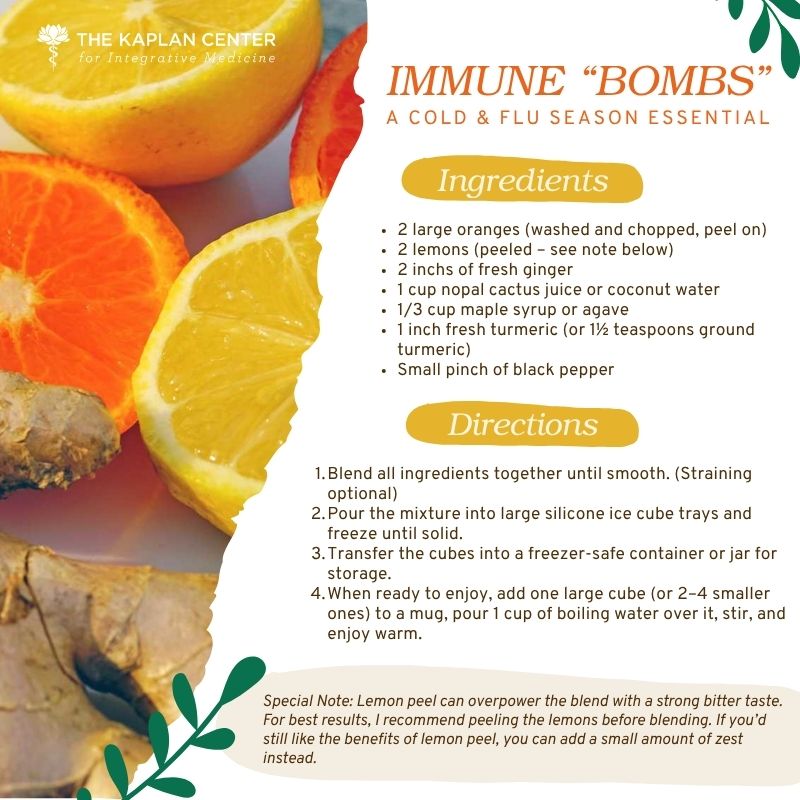
Let’s ‘Fall’ Into Wellness: A Nutritionist-Approved Immune-Boosting Recipe for Cold and Flu Season
October 13, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
PANS/PANDAS – When Sudden Symptoms Signal Something More
October 9, 2025/by Kaplan Center
Beating Burnout, A Nutritionist’s Perspective
October 1, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
3 Things That Can Happen After Stopping GLP-1s
September 11, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
What Families Need to Know About COVID and Flu Season
September 3, 2025/by Kaplan Center
September is Pain Awareness Month
September 1, 2025/by Kaplan Center
Dr. Kaplan Spoke to Northern Virginia Magazine About COVID, Flu, and Immunity — Here’s What You Should Know
August 14, 2025/by Kaplan Center
“Why Do I Feel Like Crap?”: The Overlap Between Long COVID and Perimenopause
July 30, 2025/by Kaplan Center
Why People Are Turning to EMDR (and Why You Might Want to Too)
July 23, 2025/by Kaplan CenterAre you looking to improve your overall wellness?
Personalized care you can trust.
Our integrative, non-surgical treatment approach is highly successful in maintaining wellness and also treating chronic pain and illness. For more than 30 years, we have delivered superior, cutting-edge health care in the Washington, DC area.
QuickLinks
Contact Information
Tel: 703-532-4892
Fax: 703-237-3105
6829 Elm Street, Suite 300
McLean, Virginia 22101
Map It
Hours of Operation
Mon – Thu : 8 am – 5 pm, ET
Fri : 8 am – 12 pm, ET
Food and Mood – These Dietary Recommendations are Positively Uplifting!
/in Nutrition/by Kaplan CenterThe connection between nutrition and your physical health is unequivocal. Excessive sugar consumption can lead to obesity and is also linked to inflammation and other chronic diseases such as diabetes; a high intake of unhealthy trans-fats increases your risk of future cardiac events; deficiencies in essential vitamins can accelerate cellular degeneration, thereby heightening your susceptibility to cancers and other serious illnesses. While these connections may appear simplified, their validity is well-supported by scientific evidence.
Yet despite the growing body of research illustrating the connection between a nutritious diet and enhanced mood and cognitive function, your dietary habits are often disregarded as a factor contributing to your emotional distress.
Research is increasingly confirming that inflammation of the central nervous system is a key factor in many chronic conditions, including mental health disorders such as anxiety, depression, and more severe disorders such as Major Depressive Disorder. Eating foods that are high in sugar and saturated fats can elevate inflammatory markers in your body and impact mental health by exacerbating anxiety, depression, and mood fluctuations. Dietary changes aimed at reducing inflammation and oxidative stress, as well as enhancing the gut microbiome — crucial for nervous system development and function — can substantially enhance your mental well-being.
If you would like to discuss strategies on how to improve your nutritional intake to optimize your mental and overall health, please give us a call today at 703-532-5892. We use a functional medicine approach to treatment; our goal is to treat the “whole you” so that all areas of your health are improved.
In the meantime, as the old saying goes, “you are what you eat,” so with your emotional wellbeing in mind, here are some dietary tips on how you can improve your mood and mental health.
1. Incorporate more foods rich in B-vitamins (B12, B6, Folate).
B-vitamins are involved in a number of important processes in the brain: they support cellular energy production, proper functioning of the nervous system, red blood cell formation, DNA formation, and the regulation of hormones. Studies show that deficiencies in certain B vitamins can result in an increased risk of depression.
Foods rich in B vitamins include beans, lentils, raw spinach, asparagus, romaine lettuce, broccoli, avocado, fish, shellfish & eggs.
2. Talk to us about supplements.
Even if you think you have a relatively healthy diet, supplements can provide additional support to your immune system and lower your risk of developing a host of inflammatory conditions, including depression.
Vitamin D (serotonin synthesis), vitamin C, magnesium (stress support), vitamin E (mood regulation), CoQ10, glutathione, and Omega-3 are additional examples of supplements with clinical applications in depression, anxiety and other mental health disorders.
3. Eat foods that provide gut support.
One of the many neurotransmitters used by the brain is serotonin. Among its many functions, serotonin is involved in regulating mood. We now know that as much as 95% of serotonin is produced in the intestines so maintaining the integrity of your gut microbiome with a proper balance of good and bad bacteria will help keep the production of serotonin in balance as well.
Regularly eating foods like fermented vegetables, sauerkraut, miso, and bone broth will keep your gut microbiome stocked with good bacteria.
4. Eat high protein foods at every meal to support neurotransmitter production.
Your body produces neurotransmitters by utilizing nutrients in the food you eat, primarily amino acids. For example, serotonin is a byproduct of the amino acid tryptophan; noradrenaline is made from the amino acid tyrosine, which is also converted to dopamine. Serotonin, noradrenaline (aka norepinephrine) and dopamine belong to a group of neurotransmitters called monoamines that play a major role in mood & cognitive function.
High protein foods like raw nuts, cold water fish, beans, and eggs, consumed on a regular basis, will ensure that your body is getting enough of the building blocks it needs to produce these important chemical messengers that will keep your mood stabilized.
5. When snacking, always balance carbs with fats and protein.
Keeping your carbohydrate and protein intake in balance will help stabilize mood and mental clarity and while avoiding the peaks and valleys of blood sugar levels that can also lead to other serious conditions like insulin resistance and pre-diabetes.
What does a complete protein and carb combination look like? Try combinations like: hummus with celery, bell peppers and/or carrots; apple, pear, or banana with almond butter (or any nut butter); sunflower seeds and raisins. For more combinations, click here.
6. Saffron and turmeric may support people with anxiety & depression.
Foods with turmeric and saffron have for ages been eaten for medicinal support. A study published in Journal of Affective Disorders, reported that a treatment of curcumin (the active ingredient in turmeric) and saffron were effective at easing anxiety and depressive symptoms in people with major depressive disorder.
The anti-inflammatory and antioxidant properties in turmeric and saffron help calm inflammation. Add them to your foods for flavor and anti-inflammatory benefits.
While more severe mental health conditions may necessitate treatments such as psychotherapy and medication, especially if your emotional well-being poses a risk of harm to yourself or others, your diet remains as an effective healing resource. When complemented by other strategies that address inflammation, such as exercise, meditation, and stress-reduction techniques, the result can be a brighter and more positive perspective on your life.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
References:
Gorbachev D, Markina E, Chigareva O, Gradinar A, Borisova N, Syunyakov T. Dietary Patterns as Modifiable Risk Factors for Depression: a Narrative Review. Psychiatr Danub. 2023 Oct;35(Suppl 2):423-431. PMID: 37800271.
Ma Q, Xing C, Long W, Wang HY, Liu Q, Wang RF. Impact of microbiota on central nervous system and neurological diseases: the gut-brain axis. J Neuroinflammation. 2019 Mar 1;16(1):53. doi: 10.1186/s12974-019-1434-3. PMID: 30823925; PMCID: PMC6397457.
Marx W, Moseley G, Berk M, Jacka F. Nutritional psychiatry: the present state of the evidence. Proc Nutr Soc. 2017 Nov;76(4):427-436. doi: 10.1017/S0029665117002026. Epub 2017 Sep 25. PMID: 28942748.
Petridou ET, Kousoulis AA, Michelakos T, Papathoma P, Dessypris N, Papadopoulos FC, Stefanadis C. Folate and B12 serum levels in association with depression in the aged: a systematic review and meta-analysis. Aging Ment Health. 2016 Sep;20(9):965-73. doi: 10.1080/13607863.2015.1049115. Epub 2015 Jun 8. PMID: 26055921.
Elizabeth Lipski, Digestive Wellness: How to Strengthen the Immune System and Prevent Disease through Healthy Digestion, 3rd ed. (New York: McGraw-Hill, 2004)
Roth W, Zadeh K, Vekariya R, Ge Y, Mohamadzadeh M. Tryptophan Metabolism and Gut-Brain Homeostasis. Int J Mol Sci. 2021 Mar 15;22(6):2973. doi: 10.3390/ijms22062973. PMID: 33804088; PMCID: PMC8000752.
Lopresti AL, Drummond PD. Efficacy of curcumin, and a saffron/curcumin combination for the treatment of major depression: A randomised, double-blind, placebo-controlled study. J Affect Disord. 2017 Jan 1;207:188-196. doi: 10.1016/j.jad.2016.09.047. Epub 2016 Oct 1. PMID: 27723543.
Living in the Shadow of COVID-19: The Persistent Struggle with Long-COVID
/in COVID-19, Long Covid/by Kaplan CenterIf you or someone you know has overcome COVID-19, there may be an expectation that life will quickly return to normal. Yet, for millions globally, that recovery is marred by the onset of Long-COVID, a perplexing condition that shadows them long after the virus has subsided. This condition isn’t just a continuation of the initial illness; it’s a new, often more complex battle characterized by various symptoms that weave unpredictably through every aspect of daily life.
Long-COVID, also known as Post-Acute Sequelae of SARS-CoV-2 infection (PASC), emerges as a series of physical and psychological challenges that can persist for months or even years. Imagine waking up every day not knowing which version of yourself you’ll confront—will it be a day marred by crippling fatigue, or will brain fog cloud your thoughts and hamper your simplest tasks? Perhaps breathlessness will tighten its grip during a short walk from your bed to the kitchen, or maybe today is when your heart races with unsettling palpitations that no amount of calming can ease.
These symptoms of Long-COVID, not only disrupt personal health and well-being but also affect relationships, professional ambitions, and the very essence of what it means to feel normal. In this article, we delve into the lives of those grappling with Long-COVID, exploring their daily challenges and the broader implications of a condition as varied as unpredictable. Through their stories, we seek to foster understanding and empathy, offering a glimpse into the enduring impact of a global pandemic that continues to redefine health landscapes and personal narratives alike.
Understanding Long-COVID
Long-COVID, or Post-Acute Sequelae of SARS-CoV-2 infection (PASC), is a complex, multifaceted condition that continues to baffle the medical community. It occurs after the acute phase of a COVID-19 infection and can persist for months or even years, with symptoms that can severely impact a person’s quality of life. Unlike the initial infection, which is usually confined to respiratory symptoms, Long-COVID has a broad spectrum of signs and symptoms affecting multiple organ systems.
The Scope of Symptoms
The symptoms of Long-COVID are diverse and often debilitating. They include, but are not limited to:
What We Know So Far
Research into Long-COVID is robust and diverse, addressing the varied manifestations of the condition across different patient populations. One leading theory suggests that the virus may cause a prolonged immune response, leading to widespread inflammation that affects multiple organ systems. Supporting this, Dr. Bruce Patterson’s research provides significant insights into the immunological aspects of Long-COVID. His studies have identified specific biomarkers that correlate with various Long-COVID symptoms, suggesting that certain immune cells may continue to drive inflammation well after the initial infection has resolved.
Another area of Dr. Patterson’s research focuses on the possibility that the virus may remain in some small reservoirs within the body, reactivating periodically and causing symptoms. This theory could explain the relapsing-remitting nature of Long-COVID, where symptoms flare up and subside, challenging the recovery process.
Epidemiologically, Long-COVID appears to affect around 10% to 30% of those who contract COVID-19, including those who had mild cases or were asymptomatic during the initial infection phase. The condition does not discriminate, affecting individuals young and old, healthy and those with pre-existing conditions. Dr. Patterson’s ongoing work aims to delineate further the risk factors and mechanisms underlying these disparities, providing a clearer picture of who is most at risk and why.
Dr. Patterson’s innovative approach involves using advanced diagnostic tools to better understand the “Long hauler” phenotype. His team uses sophisticated lab techniques to measure the levels of cytokines and other immune markers in patients diagnosed with Long-COVID. This research not only helps in understanding the pathophysiology of Long-COVID but also assists in developing targeted therapies that address the specific biological mechanisms at play.
This ongoing research is crucial as it continues to fill the gaps in our understanding of Long-COVID, paving the way for new treatments and interventions that are grounded in solid scientific evidence. The hope is that these efforts will lead to significant breakthroughs in the management and treatment of Long-COVID, offering relief and recovery to millions affected worldwide.
Diagnostic Challenges
Currently, no single test can diagnose Long-COVID, which complicates healthcare providers’ ability to understand and treat this condition. Diagnosis is primarily based on patient history and a process of exclusion, where other potential causes for the symptoms are ruled out.
As the scientific community’s understanding of Long-COVID evolves, it becomes clear that this is not merely a singular health issue but a spectrum of conditions with potentially profound implications for public health systems globally.
The Challenges of Working with Long-COVID
For many, the workplace becomes a battleground where daily victories hinge on health fluctuations and the understanding of colleagues and employers. Accommodations such as modified work hours, telecommuting options, and physical support can be crucial for maintaining employment and dignity.
Beyond the workplace, Long-COVID affects social interactions and personal relationships. Activities that were once routine can become exhausting or impossible, leading to social isolation and emotional strain. Support groups and online communities have become vital, providing spaces for sharing experiences and coping strategies.
Understanding Long-COVID is just the beginning. It’s crucial for everyone—employers, family members, healthcare providers—to learn how to support those affected. By raising awareness and advocating for better care and accommodations, we can improve the lives of those dealing with Long-COVID.
Medical and Supportive Care
Addressing Long-COVID requires a multifaceted approach due to its complex and varied symptoms. The Kaplan Center for Integrative Medicine has been at the forefront of treating Long-COVID by employing a personalized and integrative strategy that reflects the center’s deep understanding of chronic illness management. This approach is designed not only to alleviate the wide range of Long-COVID symptoms but also to enhance the overall well-being of each patient.
Comprehensive Treatment Modalities
At the Kaplan Center, treatment plans for Long-COVID are tailored to each patient’s individual needs. Recognizing that Long-COVID can affect virtually any system in the body, the center utilizes a variety of therapeutic modalities:
Expertise in Chronic Illness Management
The Kaplan Center’s approach is deeply rooted in its decades-long expertise in managing chronic illnesses. The center’s team includes specialists across various fields who collaborate to address the unique aspects of Long-COVID. Cutting-edge diagnostic tests developed under the guidance of experts like Dr. Bruce Patterson help pinpoint specific biomarkers. This precision medicine approach ensures that treatments are not only targeted but also more effective in managing the condition.
Patient-Centered Care
Central to the Kaplan Center’s philosophy is a patient-centered approach, where treatments are adjusted based on continuous feedback and monitoring of the patient’s progress. This dynamic approach helps in accommodating the changing nature of Long-COVID symptoms, ensuring that each patient receives care that is adapted to their evolving needs.
By integrating these various modalities and expertise, the Kaplan Center strives to provide a comprehensive treatment framework that addresses the physical, mental, and emotional challenges posed by Long-COVID. The goal is not just symptom management but enabling patients to achieve and maintain their best possible health after experiencing COVID-19.
Are you or someone you know affected by Long-COVID? Sharing your story can inspire change and help others feel less alone. Join us in spreading awareness and pushing for better support by sharing this article and your experiences on social media.
Long-COVID Recovery Services
If you are experiencing symptoms beyond six weeks of being diagnosed with COVID-19, learn more about our Long-COVID Recovery Services to regain your strength, energy, and vitality. Click here for more information.
Special Report: Understanding Long-COVID Syndrome
In this Special Report, we cover:
CLICK HERE TO GET YOUR COPY
Is a Plant-Based Diet the Key to Solving My Digestive Disorders?
/in Digestive Issues, Nutrition/by Kaplan CenterPlant-based diets are on the rise primarily due to the increasing recognition of their health benefits and better nutritional intake. As research continues to highlight the positive impacts of a plant-based diet on health and well-being, you may be among the many who are considering switching to this dietary approach.
When we talk about plant-based, you might only think “vegan” or “vegetarian,” but today there are many more types to consider, depending on your health profile. As a general rule, if you’re eating plant-based that means you are not eating meat or dairy products, eggs, poultry, or seafood. But as you’ll see from the list below, there are many ways to approach it, including keeping small amounts of meat and dairy in your diet but making an effort to add more plant-based food sources.
Plant-based diets include:
The growing availability of plant-based options in stores and restaurants makes it much easier for you to adopt; but can a plant-based diet solve your digestive disorders?
Digestive Disorders and The Impact of Plant-based Diets
Digestive disorders such as Crohn’s disease, ulcerative colitis, or irritable bowel syndrome can significantly impact your quality of life. The ongoing nature of these conditions means that symptoms of discomfort and pain can disrupt your day-to-day activities and routine tasks. If you’re struggling with digestive issues, you may be wondering if changing your diet could help, especially since a plant-based diet comes with many benefits. The following factors highlight why a plant-based diet might be an idea worth trying.
Plant-based diets tend to have a high fiber content. Fiber is essential for maintaining regular bowel movements and preventing constipation, a common digestive symptom. Incorporating more plant-based foods into your diet will result in increased fiber consumption and, by association, may improve digestion with more regular bowel habits. It is important to note there are 2 different types of fibers. Soluble and insoluble fibers are primarily found in fruits, vegetables, and whole grains. Soluble fiber attracts water, binds to fatty deposits (cholesterol), and eliminates them from the body. Insoluble fiber adds bulk to stool and helps to move food through the gut.
Studies show that chronic inflammation in the digestive tract can contribute to various digestive disorders. Adopting a plant-based diet limits or restricts pro-inflammatory foods (processed sugars and foods high in trans and saturated fats) giving the gut a chance to heal. By eating more foods high in healthy omega-3 fatty acids (which we don’t always get enough of), you’ll also be keeping the omega-3 / omega-6 ratio in balance. Plant-based foods are also naturally anti-inflammatory thanks to their abundance of antioxidants, phytonutrients, and fiber. The anti-inflammatory properties in fruits and vegetables may not only reduce the risk of developing a digestive disorder but may protect against other chronic inflammatory diseases as well.
The gut microbiome plays a crucial role in our digestive health. It does everything from nutrient absorption to boosting immune function. Research suggests that adopting plant-based diets increases the number of beneficial bacteria in our gut. How? Many plant-based foods are prebiotics and prebiotics are known to feed beneficial gut bacteria and help to promote the accumulation of healthy probiotics in the gut.
Some people have a problem breaking down the fats and proteins in animal byproducts. This can lead to increased inflammation and gut disturbances that can lead to chronic inflammation and chronic constipation in some cases. High intake of animal byproducts can lead to IBD and constant exposure can lead to colon cancer.
Incorporating More Plant-Based Foods Into Your Dietary Habits
Now that we’ve mentioned some benefits of a plant-based diet, here are a few tips on how to start.
Transitioning to a plant-based diet may improve your digestive disorders and reduce the severity of symptoms that you experience. To discuss the benefits of starting a plant-based diet, the best way to go about it, and other nutritional advice that might help improve the presence of digestive symptoms, please call us at 703-532-4892 and make an appointment.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
References
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2