
5 Ways We Can Keep Your Immune System Strong
December 10, 2025/by Kaplan Center
Want to Take Your Workout to the Next Level Next Year? These Tips Can Help
December 8, 2025/by Kaplan Center
Dr. Kaplan’s Dos and Don’ts of the Holiday Season
December 3, 2025/by Kaplan Center
Let’s Talk Webinar – A Root Cause Q&A
December 2, 2025/by Kaplan Center
Navigating Holiday Meals with Gut Issues: Simple Tips for a Comfortable Season
December 1, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
Craniosacral Therapy for TMJ | Say Goodbye to the Daily Grind
November 19, 2025/by Patricia Alomar, M.S., P.T.
From Compassionate Care to Personal Healing: A Letter to My Patients
November 18, 2025/by Kaplan Center
8 Steps to a Healthier Gut—and a Longer, Healthier Life
November 18, 2025/by Kaplan Center
Mid-Life Irritability & Fatigue Improved by Hormonal Balancing
November 13, 2025/by Lisa Lilienfield, MD
From Challenges to Change: Dr. Kaplan on Healthcare’s Biggest Challenges
October 29, 2025/by Kaplan Center
Overlooked Dangers of Mold Exposure and How to Stay Safe – Dr. Kaplan Talks to WUSA9
October 27, 2025/by Kaplan Center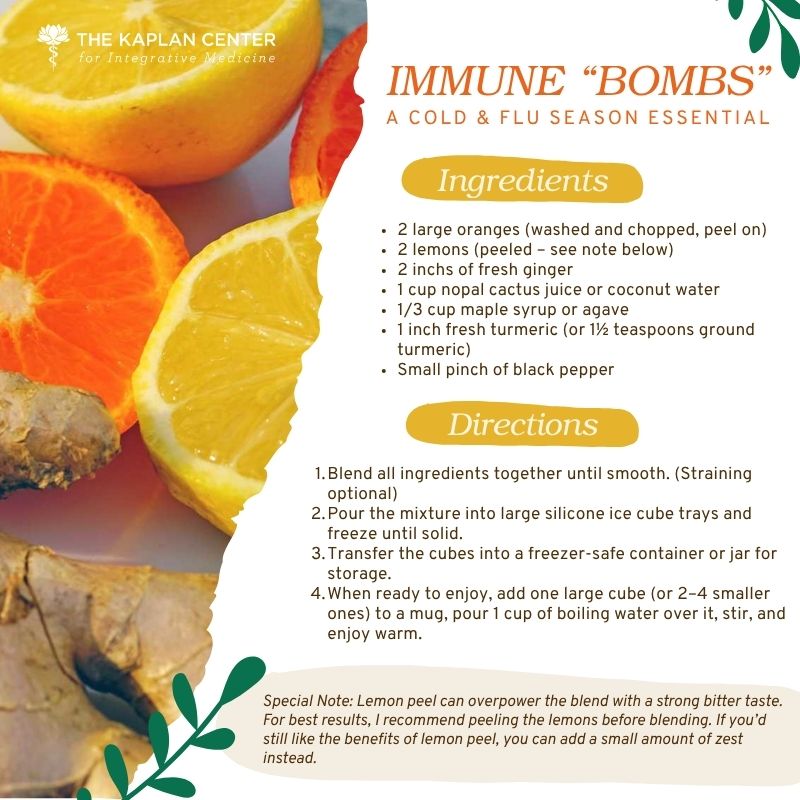
Let’s ‘Fall’ Into Wellness: A Nutritionist-Approved Immune-Boosting Recipe for Cold and Flu Season
October 13, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
PANS/PANDAS – When Sudden Symptoms Signal Something More
October 9, 2025/by Kaplan Center
Beating Burnout, A Nutritionist’s Perspective
October 1, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
3 Things That Can Happen After Stopping GLP-1s
September 11, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
What Families Need to Know About COVID and Flu Season
September 3, 2025/by Kaplan Center
September is Pain Awareness Month
September 1, 2025/by Kaplan Center
Dr. Kaplan Spoke to Northern Virginia Magazine About COVID, Flu, and Immunity — Here’s What You Should Know
August 14, 2025/by Kaplan Center
“Why Do I Feel Like Crap?”: The Overlap Between Long COVID and Perimenopause
July 30, 2025/by Kaplan Center
Why People Are Turning to EMDR (and Why You Might Want to Too)
July 23, 2025/by Kaplan CenterAre you looking to improve your overall wellness?
Personalized care you can trust.
Our integrative, non-surgical treatment approach is highly successful in maintaining wellness and also treating chronic pain and illness. For more than 30 years, we have delivered superior, cutting-edge health care in the Washington, DC area.
QuickLinks
Contact Information
Tel: 703-532-4892
Fax: 703-237-3105
6829 Elm Street, Suite 300
McLean, Virginia 22101
Map It
Hours of Operation
Mon – Thu : 8 am – 5 pm, ET
Fri : 8 am – 12 pm, ET
How to Improve AFib Symptoms
/in Conditions, Treatments, Wellness/by Kaplan CenterNutrition and other lifestyle modifications can have a meaningful influence on your Afib symptoms.
AFib, atrial fibrillation, is a form of arrhythmia (irregular heartbeat) that involves the upper chambers of the heart (atria). When the upper chambers are out of sync with the bottom chambers (ventricles) a person will experience an irregular heartbeat. AFib is the most common type of arrhythmia, affecting approximately 2.5 million adults in the United States, and unfortunately, that number is expected to rise.
Causes and Symptoms
Within the tissue of the heart, there is an electrical system that controls how the heart pumps. Most commonly, AFib is a result of damage to the heart tissue which may be caused by a condition like high blood pressure, obesity, type 2 diabetes, or an existing heart condition. It may also be caused by infection, aging, or genetics.
Between 10-40% of people with AFib are asymptomatic (“silent AFib”), but those who are symptomatic may experience any of the following:
Untreated AFib can lead to an increased risk of blood clots, stroke, and heart failure or may even complicate other health conditions; therefore, it’s extremely important to have a discussion with your provider if you are experiencing symptoms or believe you may have AFib.
Suggested Lifestyle Modifications to Lower Risk of AFib
If you have been diagnosed with Atrial Fibrillation, management may involve medicine or, when necessary, a medical procedure called ablation; however, living a healthy life with AFib will always require lifestyle changes.
Nutrition
Research confirms that a healthy diet can reduce AFib symptoms:
Mediterranean diet is rich in phytochemicals, antioxidants, and healthy fats, all of which help lower overall inflammation and keep the immune system strong.
Obesity
Obesity is a known risk factor for AFib; the good news is that it can be improved by weight loss. A study in the J American College of Cardiology found that sustained weight loss can improve AFib symptoms six-fold in patients who lost more than 10% of their body weight.
If you are having difficulty losing weight, consider working with a nutritionist or healthcare provider who can implement a personalized nutrition program to help you safely and effectively reach your goals.
Sleep apnea
There is a strong association between obstructive and central sleep apnea and Atrial Fibrillation. Sleep apnea can add an inordinate amount of stress on the body, including the cardiovascular system. A 2021 study found that people with sleep apnea are 2-4 times more likely to develop AFib. If you have sleep apnea talk to your provider about treatments to help you manage symptoms, which may include lifestyle changes, acupuncture, a customized mouthpiece, or CPAP machine. This is especially important if you have been diagnosed with AFib. This study also showed that patients who underwent ablation to improve AFib symptoms had greater success (i.e. less symptom recurrence) if their sleep apnea was previously treated.
Smoking
Much like alcohol, nicotine is a stimulant that can increase heart rate and blood pressure. A 2018 review of research found that cigarette smokers have a 32% increased risk of developing AFib compared to non-smokers, but that quitting can lower that risk. Studies that look at e-cigarettes are not as plentiful yet, but preliminary research confirms an association; this 2022 study found that e-cigarette aerosols can increase arrhythmia in mice. A long-standing smoking habit can be hard to break, but it’s never too late to quit and the benefits make it well worth the effort.
Bottom line
Your heart is too important to ignore. Living a long, active, and healthy life with AFib is possible with the risk-factor modifications mentioned above. If you feel overwhelmed by the changes you need to make, consider working with a healthcare professional who can help you set goals that are realistic and achievable; your heart will thank you.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
Platelet Rich Plasma (PRP) and Prolotherapy – Non-surgical Treatments for Musculoskeletal Pain
/in Treatments/by Kaplan CenterIf you have suffered from chronic joint pain or a sports injury to a ligament or tendon, PRP (Platelet Rich Plasma) and Prolotherapy, regenerative injection therapies that promote repair and self-healing naturally, may be a treatment option for you. There are different levels of joint dysfunction. There are also different levels of treatment. The right injection therapy can help you increase function, decrease pain and healing time, and get you back to living your best life faster. Injection therapies also help some people avoid orthopedic surgery! Regenerative injections can also be used to rejuvenate aging skin and regrow hair.
PRP – Platelet Rich Plasma
Platelet-rich plasma is an injection procedure that uses concentrates from your own blood, the platelet-rich portion of your plasma, to help your body heal and regenerate naturally. Platelets are very small cells in your blood that are involved in the clotting and healing process. When injected into the damaged area, PRP causes a mild inflammation that triggers a healing cascade. As the platelets organize in the treatment area, they release a number of enzymes to promote healing and tissue responses, including attracting stem cells and releasing growth factors to repair damaged tissue. As a result, new collagen and elastic fibers begin to develop. As the collagen matures, it begins to shrink, causing a tightening and strengthening of the tissue in the damaged area.
Prolotherapy
Prolotherapy is a safe and simple regenerative medicine injection treatment used to strengthen weak and damaged ligaments and tendons due to chronic injury or overuse. Many patients with stretched, torn, or injured ligament and joint attachments have difficulty returning to pre-injury level of functioning due to limited blood supply to these structures. Chronic anti-inflammatory/ NSAID use or overuse of steroid injections further impairs this process. Surgery can often produce scarring and a limited range of motion without addressing the root cause of dysfunction. The technique requires injection of Dextrose or Ascorbic Acid (Vitamin C), and methylcobalamin (Vitamin B12) precisely into the site of pain or injury, where the ligament or tendon attaches to the bone, joint capsule, trigger point, or inside joint.
Prolotherapy creates a mild, controlled inflammation that stimulates the body to lay down collagen with the formation of new tendon, ligament, and cartilage, resulting in a strengthening of the weakened structure. This injection process stimulates the body’s natural wound repair process. A typical treatment course is 3-6 series of injections, given every 3-4 weeks. Prolotherapy has been used for over 60 years with numerous case reports and an increasing number of controlled studies showing its effectiveness.
Physical Conditions that Can Benefit from Injection Therapies:
The best way to find out if you are a good candidate for either PRP or prolotherapy is to receive a comprehensive evaluation to rule out other possible causes of your pain (through appropriate medical testing) and to provide you with an accurate diagnosis first before recommending the most effective treatment.
If you have any of the conditions mentioned above and are looking for a non-surgical treatment option to treat your condition, please give us a call today to schedule your appointment.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
References:
Bae G, Kim S, Lee S, Lee WY, Lim Y. Prolotherapy for the patients with chronic musculoskeletal pain: systematic review and meta-analysis . Anesth Pain Med (Seoul). 2021 Jan;16(1):81-95. doi: 10.17085/apm.20078. Epub 2020 Dec 16. PMID: 33348947; PMCID: PMC7861898.
Everts P, Onishi K, Jayaram P, Lana JF, Mautner K. Platelet-Rich Plasma: New Performance Understandings and Therapeutic Considerations in 2020. Int J Mol Sci. 2020 Oct 21;21(20):7794. doi: 10.3390/ijms21207794. PMID: 33096812; PMCID: PMC7589810.
Managing Fibromyalgia Pain
/in Conditions/by Lisa Lilienfield, MDCharacterized by widespread pain, fatigue, and cognitive difficulties, fibromyalgia (FM) is a complex disorder of the central nervous system (CNS). It affects the brain’s messaging system causing those who have it to experience heightened sensitivity to pain. A fibromyalgia flare-up can last for months at a time and cause debilitating physical and emotional distress. Symptoms can vary from person to person and often suggest other conditions, making it a very difficult diagnosis. Despite all that has been learned about fibromyalgia over the last two decades, people with FM can go years without a proper diagnosis.
Fibromyalgia is associated with many other conditions like Chronic Fatigue Syndrome (also known as Myalgic Encephalomyelitis), sleep dysfunction, infections like Lyme disease or E-BV (Epstein-Barr Virus), digestive problems such as SIBO (Small Intestinal Bacterial Overgrowth), or Celiac Disease and other food allergies that can cause leaky gut. It can lead to autoimmune disorders like Hashimoto’s thyroiditis or autoimmune arthropathies. People suffering from FM may also exhibit reactions to environmental toxin exposure, like mold or heavy metals, which can be diagnosed through specialty labs looking at stool, urine, breath, and bloodwork.
A functional approach to treatment
Once you receive a fibromyalgia diagnosis, there are various treatment options and lifestyle habits to consider. As a functional medicine practitioner, my approach to treating fibromyalgia is multifaceted; I look at digestion and diet, sleep, hormone imbalances, injuries (psychological and physical), infections, environmental exposures, genetics, and more.
For example, I often find that fibromyalgia is related to a deficiency in delta-wave deep sleep; medications like Xywav, which promotes deep-wave sleep have been helpful in reducing chronic pain. If you don’t get enough deep delta wave sleep your body can’t recover, and chronic pain can be an issue. (We find that this is common in those with fibromyalgia.)
A common area of pain is the cervical spine. Treatments like physical therapy, acupuncture, or injection therapies like prolotherapy, perineural injection therapy (PIT), or PRP (platelet-rich plasma) therapy may be helpful. You may also consider having your jaw evaluated for TMJ by a dentist specializing in temporomandibular joint problems, which can often cause referred pain in the head, neck, and shoulders.
Another treatment to consider is Low-Dose Naltrexone (LDN). When chronic pain is a result of neuro-inflammation (brain inflammation), LDN can help by reducing the upregulation of the microglia that cause this inflammation.
If you have leaky gut from a food allergy, then inflammation of the intestinal tract leads to nutritional deficiencies and toxicity; I’ll want to look at dietary changes and supplementation. Supplements that may be helpful include D- ribose, fish oil, glutathione, and IV magnesium with B complex and Vitamin C (also known as Myers cocktail).
Because FM affects the CNS, it can influence your experience of pain and emotional sensations; therefore it’s very important to consider my patients’ emotional health which is often not addressed in chronic pain. There are many stress-reduction therapies that can be done from the comfort of your own home including yoga, mindfulness-based meditation, breathing exercises, and even a therapy called Emotional Freedom Technique which involves tapping acupressure points and utilizing positive affirmations. However, if you feel overwhelmed by symptoms, look for a psychotherapist who specializes in working with people with chronic pain. Dealing with chronic pain is emotionally exhausting; seeking help can be a vital lifeline for many.
As with other chronic illnesses, treating fibromyalgia is not a straightforward process; it requires a multifaceted treatment approach with close collaboration to help you recover or better manage your illness.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
Additional Resources:
Consumer Guide: 18 Things You Should Know Before Choosing a Doctor to Treat Your Fibromyalgia