Crohn’s Disease & Ulcerative Colitis
Crohn’s disease and ulcerative colitis are autoimmune, inflammatory bowel diseases (IBD) that can cause a lifetime of painful symptoms. It is estimated that up to 3 million people suffer a form of IBD, affecting men and women equally. 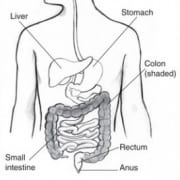
Crohn’s Disease is a chronic inflammatory disease that can affect any part of the digestive tract, but most commonly the intestines. It is associated with abdominal pain and cramping, bloating, constipation, persistent diarrhea, rectal bleeding, fatigue, unintentional weight loss, and loss of appetite. The symptoms may flare up periodically and can be mild or severe. Crohn’s Disease also can cause symptoms in other areas of the body, including skin lesions, liver inflammation, eye irritation, mouth ulcerations, and swollen joints.
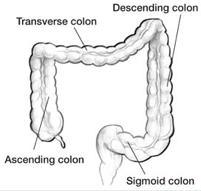
Ulcerative colitis, which shares many of the same symptoms as Crohn’s disease, differs from Crohn’s in that it is characterized by chronic inflammation of the colon only. Ulcers and inflammation always begin in the rectum and progress over time through the colon. In addition, while Crohn’s disease can affect all layers of the bowel wall, ulcerative colitis will affect only the lining of the colon.
Questions? Give Us a Call!
Both Crohn’s disease and ulcerative colitis can undermine one’s quality of life dramatically. It is not uncommon for people suffering from either of these conditions to experience feelings of hopelessness, frustration, increased stress, and anger. In some patients, these feelings can even lead to depression.
It is also important to note that although they share some symptoms with Irritable Bowel Syndrome (IBS), Crohn’s Disease and Colitis differ from IBS in that they are chronic, autoimmune diseases that can cause long-term damage to the body, including an increased risk for colon cancer. Therefore, if you are suffering with any of the symptoms described above, it is critical that you receive an accurate and timely diagnosis of your condition.
How We Can Help
At the Kaplan Center, our physicians have years of experience treating patients with chronic pain conditions, and we completely reject the notion that “you just have to live with it.”
Whether you are searching for a diagnosis for your abdominal pain, or have already been diagnosed, but have yet to find a long-lasting and effective treatment, the Kaplan Center will provide you with a treatment plan unique to your situation.
At your first visit, your Kaplan physician will take time exploring the onset of your condition, the specific nature of your symptoms and the overall status of your health. You’ll also be asked about the medications and therapies you’ve tried in the past, and what has and hasn’t worked for you. To gather additional information about your condition, specialized diagnostic laboratory testing may be necessary.
After reviewing all of the factors contributing to your condition, your physician will spend time talking with you about your diagnosis and working with you to create a customized and multi-dimensional treatment plan that addresses not only your immediate pain but also any possible underlying or co-existing conditions that may be causing or aggravating your symptoms.
We offer a multitude of effective non-surgical treatment options to help with your symptoms, including:
- Acupuncture
- Herbal Remedies & Nutritional Supplements
- Nutritional Counseling
- Prescription Medications
- Massage Therapy
- Meditation Training for Stress Management
- Biofeedback
In some extreme cases, surgery may be your best option. If this is occurs, we will coordinate with the other medical providers involved in your case and provide integrated medical care that fully supports your most rapid and complete recovery.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
Additional Resources:
Related Conditions: Celiac Disease, Chronic Abdominal Pain, Nutritional Deficiencies
Website: Centers for Disease Control and Prevention (CDC) on IBD




