
5 Ways We Can Keep Your Immune System Strong
December 10, 2025/by Kaplan Center
Want to Take Your Workout to the Next Level Next Year? These Tips Can Help
December 8, 2025/by Kaplan Center
Dr. Kaplan’s Dos and Don’ts of the Holiday Season
December 3, 2025/by Kaplan Center
Let’s Talk Webinar – A Root Cause Q&A
December 2, 2025/by Kaplan Center
Navigating Holiday Meals with Gut Issues: Simple Tips for a Comfortable Season
December 1, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
Craniosacral Therapy for TMJ | Say Goodbye to the Daily Grind
November 19, 2025/by Patricia Alomar, M.S., P.T.
From Compassionate Care to Personal Healing: A Letter to My Patients
November 18, 2025/by Kaplan Center
8 Steps to a Healthier Gut—and a Longer, Healthier Life
November 18, 2025/by Kaplan Center
Mid-Life Irritability & Fatigue Improved by Hormonal Balancing
November 13, 2025/by Lisa Lilienfield, MD
From Challenges to Change: Dr. Kaplan on Healthcare’s Biggest Challenges
October 29, 2025/by Kaplan Center
Overlooked Dangers of Mold Exposure and How to Stay Safe – Dr. Kaplan Talks to WUSA9
October 27, 2025/by Kaplan Center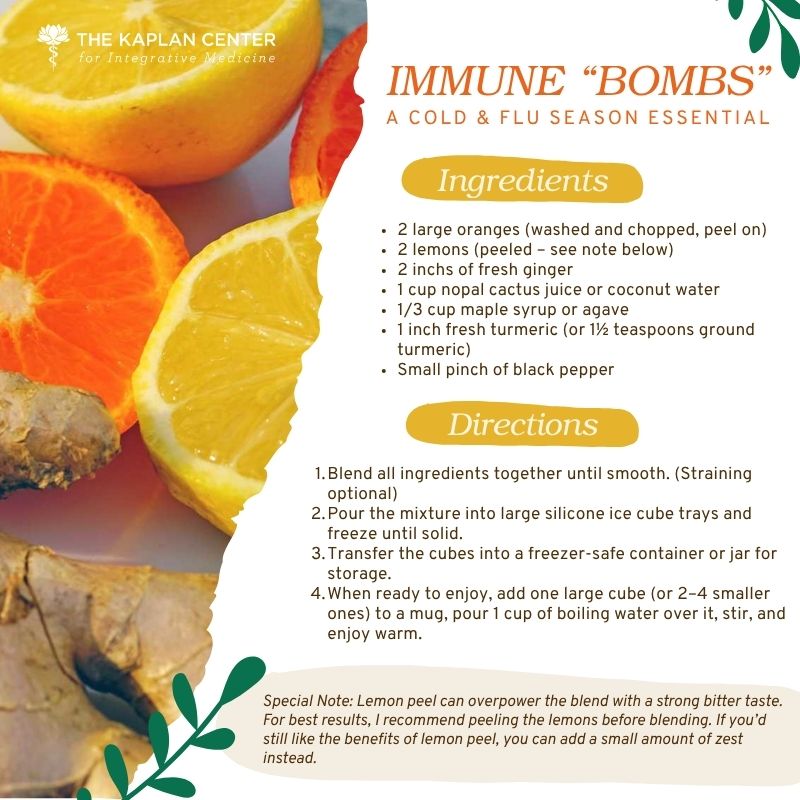
Let’s ‘Fall’ Into Wellness: A Nutritionist-Approved Immune-Boosting Recipe for Cold and Flu Season
October 13, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
PANS/PANDAS – When Sudden Symptoms Signal Something More
October 9, 2025/by Kaplan Center
Beating Burnout, A Nutritionist’s Perspective
October 1, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
3 Things That Can Happen After Stopping GLP-1s
September 11, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
What Families Need to Know About COVID and Flu Season
September 3, 2025/by Kaplan Center
September is Pain Awareness Month
September 1, 2025/by Kaplan Center
Dr. Kaplan Spoke to Northern Virginia Magazine About COVID, Flu, and Immunity — Here’s What You Should Know
August 14, 2025/by Kaplan Center
“Why Do I Feel Like Crap?”: The Overlap Between Long COVID and Perimenopause
July 30, 2025/by Kaplan Center
Why People Are Turning to EMDR (and Why You Might Want to Too)
July 23, 2025/by Kaplan CenterAre you looking to improve your overall wellness?
Personalized care you can trust.
Our integrative, non-surgical treatment approach is highly successful in maintaining wellness and also treating chronic pain and illness. For more than 30 years, we have delivered superior, cutting-edge health care in the Washington, DC area.
QuickLinks
Contact Information
Tel: 703-532-4892
Fax: 703-237-3105
6829 Elm Street, Suite 300
McLean, Virginia 22101
Map It
Hours of Operation
Mon – Thu : 8 am – 5 pm, ET
Fri : 8 am – 12 pm, ET
Let’s Talk Webinar – A Root Cause Q&A
/in Chronic Fatigue, COVID-19, Inflammation, Long Covid, Treatments/by Kaplan CenterMissed our webinar? You can still catch our insightful conversations on Long COVID and other chronic conditions — that continue to affect millions.
In these recorded sessions, our experts break down the latest understanding of symptoms, diagnosis, and treatment options, and answer real questions from participants. Whether you’re living with Long COVID, Lyme disease, ME/CFS, PANS/PANDAS—or supporting someone who is—this webinar offers insight, hope, and guidance. Watch now and learn more about these complex conditions.
Featuring Dr. Gary Kaplan, Medical Director & Founder of Kaplan Center for Integrative Medicine & author of two books, “Why You Are Still Sick” and “Total Recovery: A Revolutionary Approach to Breaking the Cycle of Pain & Depression”, and Nidhi Reva, Physician Assistant.
December 2, 2025 – THERAPEUTIC PLASMA EXCHANGE (TPE) (IMMUNE SYSTEM SERIES)
Dr. Gary Kaplan, Founder and Director of the Kaplan Center for Integrative Medicine (www.kaplanclinic.com) explains how TPE (plasmapheresis) can be used to treat a range of autoimmune, neurologic, blood disorders, and age-related conditions.
Key topics:
October 21, 2025 – LIFESTYLE & SLEEP DISTURBANCES (IMMUNE SYSTEM SERIES)
From poor sleep and chronic stress to skipped meals and late-night screen time, the habits that fill our days have a powerful impact on how our immune system performs. When those systems are constantly under strain, fatigue, inflammation, and illness can follow.
Key topics:
July 22, 2025 – WHAT’S DISRUPTING YOUR IMMUNE SYSTEM?
A weakened immune system leads to all sorts of issues, especially chronic symptoms and illness. In this webinar, Dr. Gary and Nidhi will take a deep dive into different factors that can disrupt your immune system.
Key topics:
They will also share insights on root causes to certain illnesses and tips on how to improve your immune system.
May 20, 2025 – LONG COVID
Key topics:
If you have been experiencing symptoms longer than 6 weeks after the initial onset of your symptoms and would like to speak to someone who can help, please give us a call today. We will obtain a comprehensive history, recommend complete and appropriate testing and utilize a variety of integrative medicine tools to help with recovery from the ongoing symptoms.
April 22, 2025 – LONG COVID
Key topics:
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
Navigating Holiday Meals with Gut Issues: Simple Tips for a Comfortable Season
/in Nutrition, Wellness/by Chardonée Donald, MS, CBHS, CHN, CNS, LDNThe holiday season is a time when we gather, share meals, and reconnect with the people we care about. While this time of year brings joy for many, it also carries emotional and historical complexity for others. As we celebrate, it’s important to hold space for those who may find this season challenging whether it be due to personal circumstances, health conditions, or past experiences. A moment of reflection and compassion can go a long way.
For many of us, holiday traditions revolve around food. Family recipes passed down for generations, special treats made only once or twice a year, and shared meals play a meaningful role in the festivities. However, when you’re living with gut issues or a chronic digestive condition, enjoying these foods can feel complicated. You might want to savor the flavors you love, but worry about how you’ll feel afterward.
The good news: you can still enjoy the holidays you just may need to navigate them a bit differently. Here are four helpful strategies to support your gut and your overall well-being this season:
1. Know Your Gut Status
Understanding your triggers is key. Before attending a gathering or preparing your own plate, check in with yourself. Knowing which foods your body tolerates and which ones consistently cause discomfort can help you make mindful choices without feeling deprived. Make sure to have your medications and supplements with you.
2. Respect Your Limitations
If there’s a particular dish you love, but can only handle in small amounts, give yourself permission to enjoy a little of it. Savor it slowly. Part of honoring your health is recognizing your boundaries and choosing not to push past them. Allergies and severe sensitives are exempt. Do not consume anything you are allergic to and/or can cause major bodily discomfort.
3. Put Your Fork Down Between Bites
This is something simple that can help you digest your food and connect with others. Take a bite, chew thoroughly, then set your fork down and enjoy conversation with the people around you. This naturally slows your pace, improves digestion, and gives your body time to signal fullness helping you feel satisfied without overeating.
4. Start Small
Begin with a small plate or small portions of each food. Give yourself about an hour to see how your body responds. If you’re tolerating things well, you can always return for more. Starting with large portions often leads to discomfort, feelings of shame, or feeling physically ill. Starting small gives you control.
Living with gut issues doesn’t mean you have to miss out on the joy of holiday meals. With a bit of awareness, pacing, and self-compassion, you can enjoy both the food and the company without compromising your well-being.
Enjoy and Happy Holidays!
Chardonée
Chardonée Donald is a Board-Certified Nutrition Specialist, Licensed Dietitian Nutritionist and Certified Behavioral Health Specialist. Having completed her degree requirements, Chardonée is in the final portion of her doctorate degree program in Integrative and Functional Nutrition from Saybrook University. She has a Bachelor of Science in Biomedical Science with a Minor in Nutrition and a Master of Science in Human Nutrition.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
Craniosacral Therapy for TMJ | Say Goodbye to the Daily Grind
/in Conditions, Treatments/by Patricia Alomar, M.S., P.T.Do you grind or clench your teeth at night?
Are you currently using a mouth guard, or have you been told that you may eventually need one?
Do you experience ringing in the ears, either constant or intermittent?
If you grind or clench your teeth you may also experience pain with chewing or hear a popping noise when your mouth opens or closes. Often, headaches, neck, and shoulder pain can occur.
Temporomandibular Joint Dysfunction (TMJ or TMJD) is a group of disorders that cause pain and stiffness throughout the jaw joint and surrounding muscle. In addition to the characteristic pain and stiffness in the jaw, temporomandibular joint dysfunction may cause headaches, earaches, locking or clicking of the jaw, and radiating pain throughout the face and neck.
CranioSacral therapy is a very effective, light-touch therapy that supports the body’s own healing resources to release physical imbalances and restrictions, as well as residual emotional trauma, that has been stored in the body’s membranes and connective tissue. This frees the central nervous system to perform optimally — allowing patients to experience pain relief, stronger immune function and an enhanced sense of well-being.
CranioSacral therapy helps reduce the sympathetic response in the body and helps it return to a place of balance.
CranioSacral therapy follows the osteopathic premise that if structure is normalized, function will follow. The gentle manipulation and adjusting of the cranial bones help balance the body’s system. Dr. John Upledger DO, O.M.M stated: “The temporomandibular joint (TMJ) syndrome may be primary or it may be just the tip of the iceberg. The syndrome is part of the whole person and it is the whole person that must be evaluated and treated.” Stress factors of TMJ can be physical, physiological, psycho-emotional or environmental.
CranioSacral treatment can be effective for treating hypertonicity (continual increase in the muscle tension) in the soft tissue which directly impacts the position of the temporomandibular joints (TMJ) or malocclusion (misalignment of teeth when jaws are closed). More and more dentists are realizing CranioSacral therapy can be a missing piece to a successful dental procedure.
Teeth or jaw clenching is a natural response to increased stress, chronically compressing the temporomandibular joints. If you are having pain and would like to schedule an appointment, please call 703-532-4892, Ext. 2.
Be Well, Do Good Work,
Pat Alomar, M.S., P.T.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2