
5 Ways We Can Keep Your Immune System Strong
December 10, 2025/by Kaplan Center
Want to Take Your Workout to the Next Level Next Year? These Tips Can Help
December 8, 2025/by Kaplan Center
Dr. Kaplan’s Dos and Don’ts of the Holiday Season
December 3, 2025/by Kaplan Center
Let’s Talk Webinar – A Root Cause Q&A
December 2, 2025/by Kaplan Center
Navigating Holiday Meals with Gut Issues: Simple Tips for a Comfortable Season
December 1, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
Craniosacral Therapy for TMJ | Say Goodbye to the Daily Grind
November 19, 2025/by Patricia Alomar, M.S., P.T.
From Compassionate Care to Personal Healing: A Letter to My Patients
November 18, 2025/by Kaplan Center
8 Steps to a Healthier Gut—and a Longer, Healthier Life
November 18, 2025/by Kaplan Center
Mid-Life Irritability & Fatigue Improved by Hormonal Balancing
November 13, 2025/by Lisa Lilienfield, MD
From Challenges to Change: Dr. Kaplan on Healthcare’s Biggest Challenges
October 29, 2025/by Kaplan Center
Overlooked Dangers of Mold Exposure and How to Stay Safe – Dr. Kaplan Talks to WUSA9
October 27, 2025/by Kaplan Center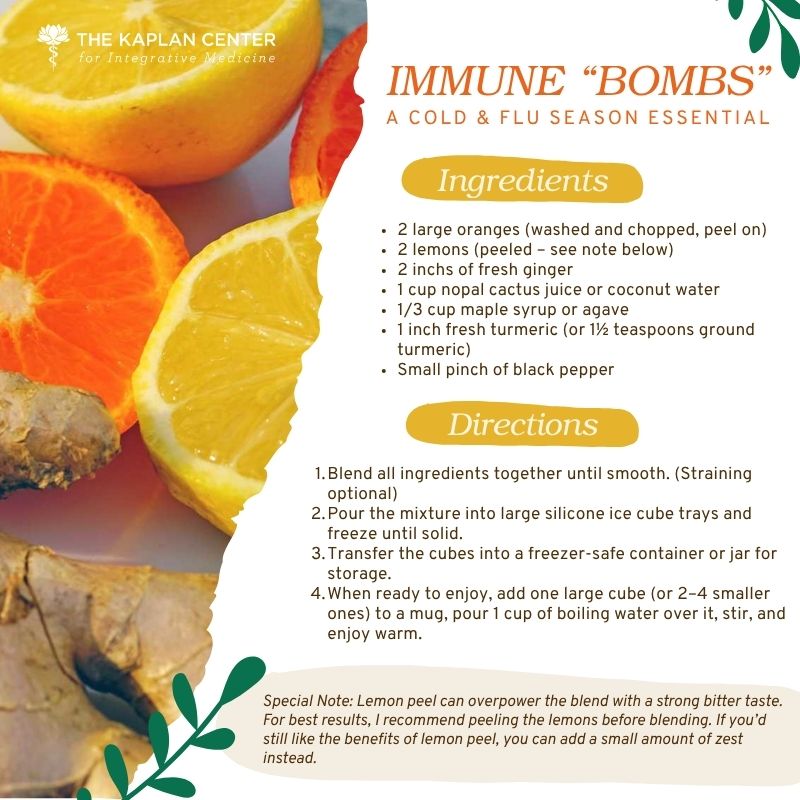
Let’s ‘Fall’ Into Wellness: A Nutritionist-Approved Immune-Boosting Recipe for Cold and Flu Season
October 13, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
PANS/PANDAS – When Sudden Symptoms Signal Something More
October 9, 2025/by Kaplan Center
Beating Burnout, A Nutritionist’s Perspective
October 1, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
3 Things That Can Happen After Stopping GLP-1s
September 11, 2025/by Chardonée Donald, MS, CBHS, CHN, CNS, LDN
What Families Need to Know About COVID and Flu Season
September 3, 2025/by Kaplan Center
September is Pain Awareness Month
September 1, 2025/by Kaplan Center
Dr. Kaplan Spoke to Northern Virginia Magazine About COVID, Flu, and Immunity — Here’s What You Should Know
August 14, 2025/by Kaplan Center
“Why Do I Feel Like Crap?”: The Overlap Between Long COVID and Perimenopause
July 30, 2025/by Kaplan Center
Why People Are Turning to EMDR (and Why You Might Want to Too)
July 23, 2025/by Kaplan CenterAre you looking to improve your overall wellness?
Personalized care you can trust.
Our integrative, non-surgical treatment approach is highly successful in maintaining wellness and also treating chronic pain and illness. For more than 30 years, we have delivered superior, cutting-edge health care in the Washington, DC area.
QuickLinks
Contact Information
Tel: 703-532-4892
Fax: 703-237-3105
6829 Elm Street, Suite 300
McLean, Virginia 22101
Map It
Hours of Operation
Mon – Thu : 8 am – 5 pm, ET
Fri : 8 am – 12 pm, ET
“Why Do I Feel Like Crap?”: The Overlap Between Long COVID and Perimenopause
/in Menopause, Women's Health/by Kaplan CenterDuring a recent Kaplan webinar on the immune system—covering what happens when it becomes dysregulated and how that affects healing—one of the best questions came from a woman in her 40s. She asked, “How do I know if what I’m experiencing is Long COVID… or perimenopause?”
Honestly? It’s a great question—and a hard one. Because here’s the truth: the symptoms can look nearly identical.
Both can make you feel like your body has betrayed you—exhausted, foggy-headed, moody, anxious, and just off. A 46-year-old patient recently said it best:
“I feel like I’m dragging from the second I wake up. I forget names, lose my keys, and I’m hot all the time—then I wake up drenched in sweat. My sleep’s a mess. Sometimes I get a strange burst of energy, but then feel like I could pass out. My hair’s falling out, my nails are brittle, and no matter what I do, my midsection keeps growing.”
She looked at me and asked, “Am I sick? Or is this just getting older?”
That question sits at the center of what so many women are grappling with.
What Is Perimenopause?
Menopause is defined as 12 months without a period. Perimenopause is the hormonal lead-up—and it can last up to a decade. But it’s not a graceful winding down. It’s hormonal whiplash—a surge, then a drop, then another surge.
That rollercoaster can cause:
And too often, it’s brushed off as “just stress” or “just aging.”
Meanwhile… Long COVID Can Look Strikingly Similar
At the Kaplan Clinic, we see this daily. Long COVID can cause:
Here’s the kicker: Women ages 35 to 55—prime perimenopause years—are also among the most affected by Long COVID.
So yes, you can be navigating both. Even with normal labs.
So What’s Next?
There’s no single test that gives you a neat answer. But there is a way forward.
At the Kaplan Center, we begin with a comprehensive evaluation:
We develop a unique plan based on you, but above all else: we listen. You deserve more than vague reassurance or being handed a reflexive antidepressant.
Because so many women today are living in bodies caught between transitions: hormonal, immunological, and emotional. If this story feels familiar, you’re not alone.
Schedule an appointment. Let’s sort through the gray and help you find your way back to yourself.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
Why People Are Turning to EMDR (and Why You Might Want to Too)
/in Mental Health, Treatments/by Kaplan CenterLet’s be honest—therapy has become more normalized. Insurance often covers it, the stigma has lessened, and many of us have spent time on a couch (or a Zoom screen) working through life’s challenges.
But what if you’ve already done therapy for years? Or you’re skeptical, because talking doesn’t seem to fix what’s broken in your body?
That’s where EMDR comes in.
EMDR—Eye Movement Desensitization and Reprocessing—was developed in the late 1980s by Francine Shapiro to help veterans with PTSD. But today, it’s used far beyond classic trauma cases. Many of us walk around with unresolved stress—chronic, buried, or subtle—that keeps our nervous system stuck in fight-or-flight. And that’s a major barrier to healing.
At the Kaplan Center, we take a holistic and integrative approach to care—yes, we focus on sleep, nutrition, hormones, and toxins—but also on how your past experiences shape your body’s stress response. Because no matter how well we treat the physical layers, if the nervous system is still stuck in survival mode, progress stalls.
EMDR can be a game-changer.
EMDR or the Adaptive Information Processing (AIP) model seems to tap into your brain’s inherent ability to heal so that past experiences are processed in a more healthy way. When something overwhelming happens and your brain doesn’t fully integrate the memory, it can get “stuck” creating anxiety, triggers, even physical symptoms. EMDR helps “unstick” those memories so your nervous system can finally reset.
If you’ve read The Body Keeps the Score, you would understand: Unprocessed stress doesn’t just live in your head—it lives in your body.
So what does EMDR actually do? It helps the brain reprocess distressing memories or patterns so they’re no longer so triggering. It’s not traditional talk therapy. It’s structured, short-term, and highly effective. At our center, our therapist Jodi Brayton uses EMDR to help patients with chronic pain and illness regulate their nervous systems and finally start to recover.
So if you’re stuck in your healing journey, or you’ve done all the right things but still feel unwell, maybe it’s time to consider this therapy that works at the intersection of mind and body. Not because you’re “crazy,” but because your body is trying to heal, and sometimes it needs your brain’s help to get there.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
Research on the benefits of EMDR:
Vock S, Tesarz J. Eye movement desensitization and reprocessing (EMDR) in pain therapy: Potentials, mechanisms and clinical applications for chronic pain with traumatic background. Schmerz. 2025 Aug;39(4):278-286. German. doi: 10.1007/s00482-025-00890-w. Epub 2025 Jun 30. PMID: 40586918.
Rentinck EM, van Mourik R, de Jongh A, Matthijssen SJMA. Effectiveness of an intensive outpatient treatment programme combining prolonged exposure and EMDR therapy for adolescents and young adults with PTSD in a naturalistic setting. Eur J Psychotraumatol. 2025 Dec;16(1):2451478. doi: 10.1080/20008066.2025.2451478. Epub 2025 Jan 21. PMID: 39835632; PMCID: PMC11753006.
Novo Navarro P, Landin-Romero R, Guardiola-Wanden-Berghe R, Moreno-Alcázar A, Valiente-Gómez A, Lupo W, García F, Fernández I, Pérez V, Amann BL. 25 years of Eye Movement Desensitization and Reprocessing (EMDR): The EMDR therapy protocol, hypotheses of its mechanism of action and a systematic review of its efficacy in the treatment of post-traumatic stress disorder. Rev Psiquiatr Salud Ment (Engl Ed). 2018 Apr-Jun;11(2):101-114. English, Spanish. doi: 10.1016/j.rpsm.2015.12.002. Epub 2016 Feb 11. PMID: 26877093.
Valiente-Gómez A, Moreno-Alcázar A, Treen D, Cedrón C, Colom F, Pérez V, Amann BL. EMDR beyond PTSD: A Systematic Literature Review. Front Psychol. 2017 Sep 26;8:1668. doi: 10.3389/fpsyg.2017.01668. PMID: 29018388; PMCID: PMC5623122.
“I Kept Bracing Myself for a Crash”: A Long COVID Recovery Story
/in COVID-19, Long Covid, Wellness/by Kaplan CenterShe was referred to our clinic by someone who knows us well—her husband. A quietly observant man, he had watched his wife struggle for years with a tangled web of symptoms: daily headaches, joint pain, heart palpitations, brain fog, and a deep fatigue no nap could fix. Her mood had darkened. Her anxiety and brain fog were crippling. She was barely keeping up with her demanding job.
The worst part? She’d seen multiple specialists—most of whom dismissed her symptoms, told her to lose weight, and suggested it was all in her head.
She was 56 when she came to us. Smart, capable, and determined—but depleted and discouraged.
Her medical history was complex: a confirmed case of Lyme disease in 2009 that was poorly treated (despite a classic bull’s-eye rash she had to fight to get acknowledged), Epstein-Barr virus, sleep apnea, stage 2 kidney disease, and two previous melanomas.
COVID was the final blow that toppled her health.
She had two confirmed infections—one severe, one mild—and afterward, it felt like her body never got back up off the mat. She described feeling “inflamed all over,” with frequent diarrhea, daily headaches, short-term memory loss, difficulty concentrating, and worsening cognitive haze. Her reading and computer skills were slipping. She feared losing her job.
Still, she pushed through for two full years.
By the time she came to us, she was exhausted in every sense of the word. We followed our comprehensive, systematic approach and she was diagnosed as having a dysregulated innate immune system, persistent Lyme titers, elevated inflammatory markers, and occipital neuralgia.
We built a layered treatment plan focused on gut health, sleep, immune modulation, and cognitive recovery. It wasn’t quick—but it worked.
She began to stabilize.
Then came the real test: Italy. A nine-day trip with her family this summer. She was excited, but apprehensive. “I kept bracing myself,” she told us. “I thought, I’m going to crash today. I’m going to crash.”
But she didn’t.
Day after day, she woke up and wandered through Italian towns in 90-degree heat. She climbed the Torre degli Asinelli – 498 steps to the top—without getting winded. She walked 20,000 steps a day.
Two years ago, she couldn’t walk from her car to a coffee shop without needing to rest for hours. Now, she was exploring the world again—with joy and energy.
“I felt amazing,” she said. “My energy is a 9 out of 10.”
We recently rechecked her Lyme labs. They’re still positive. And yes, she was frustrated. Rightfully so—she did everything she was supposed to do back then, and it still wasn’t enough. But her cytokine panel looks better. Her immune system is recovering. And most importantly, she feels like herself again.
She’s hopeful. And she’s a believer in the Kaplan Method™.
The systematic approach we use here is what medicine should be. Our method starts by recognizing that immune system dysfunction is often at the root of chronic illness. We look beyond symptoms to understand how early life experiences, family dynamics, environmental triggers, and nervous system imbalances shape a person’s ability to heal. Our team—including acupuncturists, psychotherapists, physical therapists, and nutritionists—works collaboratively to create personalized care plans focused on resilience and recovery.
She’s one of the most grateful people we’ve ever treated. Bright, thoughtful, kind, and always curious about how her body works. It’s been a privilege getting to know her—and her family.
Sometimes, healing begins when you stop bracing for the crash—and start climbing.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2