When Going Gluten-free Makes Sense
Gluten is a general name for the family of proteins found in the grains wheat, barley, and rye. Glutenin and gliadin, the 2 main proteins in gluten, are responsible for giving dough its characteristic elasticity and glue-like structure before the baking process and its wonderful texture and rise when baked.
Most people can eat gluten without any problem. However, for some, even the smallest amount of gluten can trigger a wide array of inflammatory reactions in the body when consumed, with symptoms sometimes lasting for months. Sensitivity to gluten presents across a spectrum, sometimes being the primary factor that is making a patient ill, but more often it exacerbates an existing pain condition.
Gluten is directly correlated with 3 major gastrointestinal disorders: Celiac disease (CD), non-celiac gluten sensitivity (NCGS), and wheat allergy.
Celiac disease
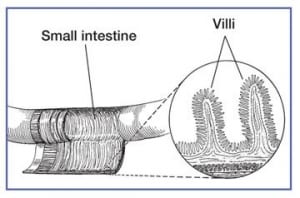
Celiac disease is an autoimmune disorder that is triggered by eating foods that contain gluten. Even miniscule amounts can trigger a reaction. Celiac disease is characterized by the damage and atrophy of the villi of the intestinal cell lining. The villi are finger-like extensions that extend from the wall of the small intestine into the lumen. The primary role of these villi is to absorb nutrients from the foods we consume. This damage leads to an increase in the space between cells, allowing food particles to enter the bloodstream (also referred to as intestinal permeability or “leaky gut”), and triggers an inflammatory immune response. CD can directly cause atopic problems, nutritional deficiencies, and anemias. Research also confirms that individuals with CD have a higher risk of developing other autoimmune disorders, such as Type 1 Diabetes, Sjogren’s Syndrome, Rheumatoid Arthritis, and Hashimoto’s thyroiditis.
Celiac disease is also genetically linked, thus, anyone with a relative who has CD is at higher risk to develop it themselves. You can be tested for celiac disease just as you can be tested for food allergies and food sensitivities.
If you have been diagnosed with Celiac disease, going gluten-free is a must. Usually, after following a gluten-free diet (GFD) for just one month the health of patients with celiac disease improves dramatically.
Non-celiac gluten sensitivity
People with non-celiac gluten sensitivity share many of the symptoms common to celiac disease but do not test positive for CD. Once gluten is eliminated from one’s diet, patients with NCGS will quickly see an improvement in several symptoms.
Wheat allergy
Wheat allergy is an allergic reaction to any number of the proteins found in wheat, not necessarily gluten. A person diagnosed with a wheat allergy must avoid eating any form of wheat to avoid triggering an immune reaction but can tolerate eating gluten found barley and rye.
Symptoms of celiac disease & non-celiac gluten sensitivity
The most common symptoms of celiac disease and gluten sensitivity are listed below. Individuals with these conditions can experience a combination of any number of symptoms and some people with CD report having no symptoms at all.
Gastrointestinal:
- Chronic diarrhea and/ or constipation
- Chronic indigestion
- Dehydration
- Irritable Bowel Syndrome
- Flatulence
- Sores or ulcers inside the mouth
- Poor appetite and lactose intolerance
- Recurring abdominal bloating, cramping, distention or pain and vomiting
Extra-intestinal:
- Anxiety and Depression
- Extremely itchy skin rash called dermatitis herpetiformis (DH)
- Fatigue
- Fluid retention
- Hair loss
- Joint pain, muscle weakness or cramping
- Migraine headaches
- Peripheral Neuropathy (tingling and numbness in hands and feet)
- Vitamin deficiencies, especially Vitamin D
- Weight loss
- Cognitive impairment
The following foods usually or often contain gluten:
- Breading, coating, Panko (Japanese breadcrumbs) (wheat)
- Cakes, pastries, cookies, pies, etc. (wheat)
- Broth, soup bases (barley)
- Brown rice syrup (barley)
- Candy, for example, licorice (wheat) and some chocolates (barley)
- Croutons (wheat)
- Breakfast cereals (wheat, barley)
- Imitation bacon (wheat)
- Imitation seafood (wheat)
- Processed lunchmeat, sausages, frankfurters (wheat)
- Marinades (wheat, barley)
- Pasta (wheat)
- Sauces, gravies (wheat)
- Self-basting poultry (wheat)
- Soy sauce or soy sauce solids (wheat, barley)
- Stuffing, dressing (wheat)
- Thickeners (roux) (wheat)
- Communion wafers (wheat)
- Herbal supplements (wheat)
- Drugs and over-the-counter medications (wheat)
- Nutritional supplements, Vitamins, and mineral supplements (wheat)
- Play-Doh (wheat)
- Beer, ale, porter, stout, malt liquor (wheat)
Behind the label
In the last several years, we have seen tremendous growth in gluten-free products available in grocery stores and restaurants, and the number of gluten-free cookbooks has grown exponentially. In 2013, the FDA required that food manufacturers who wished to use a “gluten-free” label on their products had to limit its gluten content to 20 parts per million or less. The FDA chose this standard based on evidence that suggests that most individuals with celiac disease can tolerate “variable trace amounts and concentrations of gluten in foods (including levels that are less than 20 ppm gluten) without causing adverse health effects.”
In 2020, “gluten-free” labeling requirements extended to fermented or hydrolyzed foods. The FDA’s rule requires that manufacturers themselves keep records to support the “gluten free” claim.
Going gluten-free can be tricky; federal law requires wheat and the other top food allergens (milk, eggs, fish, Crustacean shellfish, tree nuts, peanuts, wheat, sesame, and soybeans) to be clearly identified on food labels, but there are no regulations regarding barley, rye, and oats. For example, if you see a label that lists malt extract, malt vinegar, malt flavoring, or brewer’s yeast, that product will contain some barley. Learning what to look for on a food label is essential!
Do oats contain gluten?
Strictly speaking, no, but oats have been found to be at risk of contamination with gluten during its production process. Gluten-free oats are available and should be labeled as such. Many people with CD can eat a small amount of gluten-free oats without a problem. A percentage of people with CD react the same way to the protein in oats as they do to gluten.
Should you go gluten-free without a diagnosis or symptoms?
Important to note is that implementing a gluten-free diet without a Celiac diagnosis or without any symptoms of sensitivity does not come without some risk. A review published in Clinical Nutrition in 2016 found people who follow a gluten-free diet are at higher risk of developing nutritional deficiencies. The reason? Many processed gluten-free foods on the market are lower in vitamins and minerals, such as Vitamin B12, Vitamin D, folate, magnesium, iron, and calcium, than their non-gluten-free counterparts.
What can you eat on a gluten-free diet?
Plenty! In addition to all of the processed gluten-free products on the market, fruits, vegetables, meat and poultry, fish and seafood, dairy, beans, legumes, and nuts are all part of a healthy, gluten-free diet.
The following grains do NOT contain gluten: rice, corn (maize), millet, quinoa, sorghum, buckwheat, amaranth, teff, flax, chia, and nut flours.
In sum, a gluten-free diet is necessary for all patients with celiac disease and highly recommended for patients with a commonly associated autoimmune disorder (Sjogren’s disease, Hashimoto’s thyroiditis). Our experience at the Kaplan Center has also shown that patients with non-Celiac, inflammatory conditions, such as arthritis, chronic muscle pain, chronic fatigue, and fibromyalgia, also see great improvements in their health when implementing a gluten-free diet.
Learning how to dissect food labels and understanding what ingredients indicate the presence of gluten is the key to staying gluten-free! By eliminating your exposure, a GFD can provide a clean slate to curb the cycle of inflammation.
If you are experiencing some of the symptoms above and have not been able to find resolution, please give us a call and make an appointment. We’re here to help you get to the root cause of your symptoms so healing can begin. Call 703-532-4892.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2









Leave a Reply
Want to join the discussion?Feel free to contribute!