“Text Neck Syndrome” Is No Joke; Your Chronic Neck Pain is Trying to Get Your Attention
Chronic neck pain has been a growing problem since the arrival of handheld technology. “Text Neck,” also called forward head posture, is a condition caused by the repetitive stress placed on the cervical spine from looking down. In addition to chronic neck pain, bending your neck for too long may also cause upper shoulder pain, headaches, muscle stiffness and postural changes. But neck pain can also be an important clue to the existence of underlying health issues.
Looking down for an extended period of time puts you at risk of overstretching the supporting muscles, tendons, and ligaments of the cervical spine. These elastic structures should recoil back to normal, but there are many reasons why the connective tissue in the neck doesn’t rebound, including:
- Disc problems – cervical discs can wear out and start to degenerate over time, making the neck feel painful and stiff.
- Facet Arthritis – when cartilage that covers the ends of the facet joints wear out pain and stiffness can result.
- Hypermobility Syndromes – neck pain, headaches, “heavy head” are all common symptoms of cervical hypermobility.
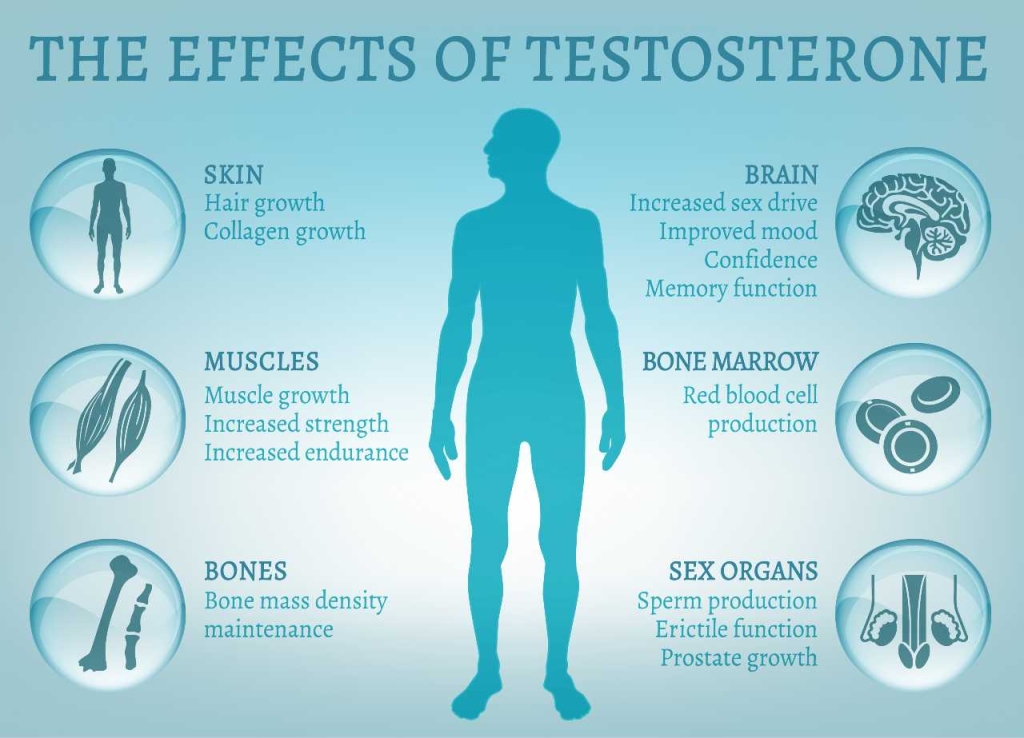
- Hormonal Changes – cervical spine (neck) problems could be an indicator of low thyroid in women and low testosterone in men
- Chronic Infection – untreated viral and bacterial infections can lead to painful inflammation of the neck muscles.
- Altered Metabolism – Chronic neck pain has also been associated with metabolic syndrome and a high body mass index.
- Nutritional Deficiencies – B12 and Vitamin D deficiencies can cause or worsen neck pain.
- Emotional Stress – Many people “carry stress” in their neck which presents as pain and can cause real physiological changes.
Diagnosing & Treating Chronic Neck Pain
At the Kaplan Center, we’ll look at multiple areas of health to determine the root cause of your pain and all the factors that may be exacerbating your symptoms. Neck problems are best treated by a multidisciplinary team and comprehensive treatment is key to long-lasting results. Depending on your evaluation and test results, recommended treatments may include:
- Osteopathic manipulation – Manual therapies are often used for treating chronic neck pain. Craniosacral therapy, visceral manipulation, myofascial release and strain/counterstrain are just a few of the techniques that we can use to rebalance and realign musculoskeletal, connective, visceral, and other body tissues to ensure optimal body function.
- Physical therapy – Chronic neck pain can often be successfully treated with physical therapy. Our physical therapists can evaluate and treat your condition with strengthening and stretching exercises, as appropriate.
- Acupuncture is thought to work by blocking pain messages to the brain with competing stimuli through the release of endorphins (the body’s natural painkillers) and the secretion of neurotransmitters, which affect one’s perception of pain.
- Hormone replacement – When hormonal changes are the cause of your pain, hormone replacement therapy can help improve symptoms for both men and women.
- Stress reduction – Mind body therapies can help lower stress.
- Nutrition & supplementation – Positive dietary changes and supplementation will help correct deficiencies and can improve your pain symptoms and overall wellbeing.
- Regenerative medicine therapies, including prolotherapy and platelet-rich plasma have been very successful in treating chronic neck pain related to texting and poor posture.
The treatments above can help relieve your immediate pain, promote long-term symptom relief, and help prevent future episodes of neck pain. In our experience, a combination of treatment strategies works best.
Don’t ignore the message, let us help you! Please give us a call today to make an appointment – 703-532-4892. Ext 2.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2