Common Links Between Thyroid Disease & Celiac Disease
If you’ve been diagnosed with either celiac disease or thyroid disease but continue to experience symptoms like fatigue, digestive issues, or unexplained pain, a co-existing autoimmune disorder at play. If you’ve been feeling “unwell,” especially for a prolonged period of time, it is important that all your body systems are carefully examined to determine if deficiencies are preventing you from getting better.
At The Kaplan Center, we prioritize your overall health, not just the symptoms. We provide a comprehensive and holistic approach to testing and treatment to ensure an expedited and accurate diagnosis, addressing all factors contributing to your condition. If you’ve struggled with chronic issues and haven’t found relief despite seeing multiple doctors, contact us today. Speak with one of our nurses to explore how we can help you on your path to better health.
Signs and symptoms of celiac disease
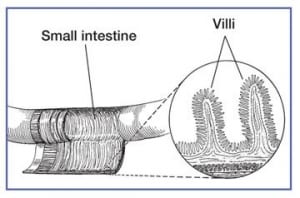
Celiac disease is an autoimmune disorder in which your body attacks and damages the lining of your small intestine when you consume gluten. Even the smallest amount can trigger an inflammatory response that targets and damages the villi, fingerlike projections whose job it is to absorb nutrients from the digested foods you eat. When villi become damaged, your body is no longer able to absorb nutrients it needs to stay healthy and malnutrition and other serious health conditions become a serious risk. Long-term consequences of celiac can include infertility and pregnancy complications, developing other autoimmune disorders, and cancer. Common symptoms of celiac disease include diarrhea, weight loss, nausea, bloating, and abdominal pain.
Because celiac disease can lead to other serious health conditions early diagnosis is key. But, because celiac shares symptoms with many other conditions, it may be years before it is detected.
Signs and symptoms of thyroid disease
If you’re diagnosed with autoimmune thyroid disease, your immune system attacks and damages the tissues of your thyroid gland, causing it to produce either too much or too little thyroid hormone. Because of the major role your thyroid gland plays in regulating your body’s mechanics, like how quickly you burn calories, your heart rate, and other vital functions, any breakdown of the thyroid gland can cause a cascade of symptoms to appear. The signs and symptoms associated with thyroid disease vary depending upon whether your thyroid is under-producing or over-producing thyroid hormone.
Hypothyroidism: Too little thyroid hormone, or hypothyroidism is the most common type of thyroid disease. It’s most often caused by the autoimmune condition Hashimoto’s thyroiditis, but it can also be caused by other factors, such as iodine deficiency. If you have hypothyroidism, your symptoms may include fatigue, a general sense of feeling cold, and dry skin and hair. You may also have elevated cholesterol levels, experience weight gain due to a decrease in metabolism, have difficulty with mental concentration (“brain fog”), or have irregular menstrual periods. People with an underactive thyroid often experience many other problems associated with weight gain including insulin resistance and diabetes, high blood pressure, and heart disease.
Hyperthyroidism: Symptoms of hyperthyroidism, too much thyroid hormone, include weight loss, enlarged thyroid (goiter), nervousness, high blood pressure, gastrointestinal problems, and a rapid heartbeat. Hyperthyroidism is most often caused by the autoimmune condition, Graves’ disease, accounting for between 60-80% of cases.
Both types of thyroid disorders may cause you to experience sleep disorders, severe fatigue, and changes in bowel habits, ranging from constipation to diarrhea. Pregnant women, whose hormone levels change dramatically to accommodate the growing fetus, may experience a variety of problems due to untreated thyroid conditions.
Co-occurrence of thyroid disease and celiac disease
Generally speaking, if you have an autoimmune condition, you are predisposed to developing other autoimmune conditions. Studies have shown that people with celiac disease are more likely to develop ATD than the general public, and the reverse is also true. This research suggests that considering and possibly testing for thyroid disorders in patients with CD – and vice versa – should become routine.
Too often medical providers become focused on one symptom or one disease process to the exclusion of other important medical evidence. In fact, the New England Journal of Medicine published a study suggesting that the #1 mistake most doctors make is narrowing the differential diagnosis – or list of possible conditions – too quickly, which limits what we’re able to see, never mind accurately diagnose and treat. It’s critical to cast a wide net in the process of diagnosing a patient, and this takes time.
Our functional medicine approach involves looking at all areas of your health to uncover imbalances or deficiencies that may be contributing to disease. When deficiencies are identified we’ll spend time talking with you about your diagnosis and working with you to create an integrative treatment plan that addresses not only your immediate symptoms but also any possible underlying or co-existing conditions that may be causing or aggravating them.
Does a gluten-free diet help thyroid antibodies?
When you have celiac disease and you remove gluten from your diet, your autoimmune antibodies return to normal, as expected. Medical research also suggests, however, that when people with celiac and thyroid disease adopt a gluten-free diet, not only do their celiac-related antibody levels improve, but often their thyroid antibody levels also decrease. This suggests that a gluten-free diet improves thyroid function, and it may mean that people with celiac who are gluten-free require less thyroid medication.
Additional therapies that focus on improving your digestive health and lowering inflammation, include
- Acupuncture
- Nutritional Counseling
- Herbal Remedies & Nutritional Supplements
- Stress Management
- Sleep Evaluation & Management
When a thyroid disorder is confirmed, hormone replacement may also be discussed as part of your treatment.
Original publication: August/2010; updated January/2017 & April/2024
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
References
https://my.clevelandclinic.org/health/diseases/8541-thyroid-disease
https://my.clevelandclinic.org/health/diseases/15244-graves-disease