Why Meditation Is One of The Most Important Things You Can Do for Heart Health: A Doctor Explains
Despite medical advances, heart disease remains the number one cause of death for both men and women in the United States. This is a startling reality, especially given how preventable it is for those of us that are not genetically predisposed. Stress, along with smoking, sedentary habits, and a poor diet are some of the main lifestyle-related risk factors that increase your chance of developing the condition.
This article looks specifically at stress as a risk factor for heart disease, and meditation as a natural and proven method to mitigate its effects.
How The Stress-Response System Works
Whether it’s related to work, health, money, relationships, or some other life event or situation, stress eventually finds its way into your life. Thankfully, your body is well equipped to handle stressful situations thanks to the autonomic nervous system (ANS). The ANS is dedicated to regulating processes such as increased heart rate and shallow breathing, which kick in when you begin to experience stress or anxiety.
The stress-reaction process is truly an amazing and efficient one: when your body is under stress the amygdala in the brain fires up and sends an alert that there is a stressor, then the sympathetic nervous system is activated and prepares your body to “fight or take flight.” Your adrenals then go to work, supplying your body with cortisol and adrenaline, completing the trifecta of the stress-response process.
Typically the stress-response system is self-limiting, and when the stressor is gone, cortisol and adrenaline levels subside, and allostasis or stability is restored to your body. However, when the stress-reaction process is repeated multiple times over a relatively short period, stress becomes chronic, and the system breaks down. This is called “allostatic load,” which often results in an increase in physiological issues that compromise your immune system, inducing illness, and even accelerating disease processes such as diabetes, cancer, and heart disease.
Questions? Give Us a Call!
Why Meditation Can Help Your Heart
The practice of meditation for stress relief has become more widely accepted as a complementary treatment to conventional medicine. As research affirms its positive psychological and physiological effects on the body, the attitude of “it can’t hurt” has shifted to “it can help.” According to an NIH survey done in 2017, next to yoga, meditation is the second most used mind-body therapy in the U.S.
How Lowering Stress Promotes Heart Health
A regular meditation practice can play a role in reducing cardiovascular disease by:
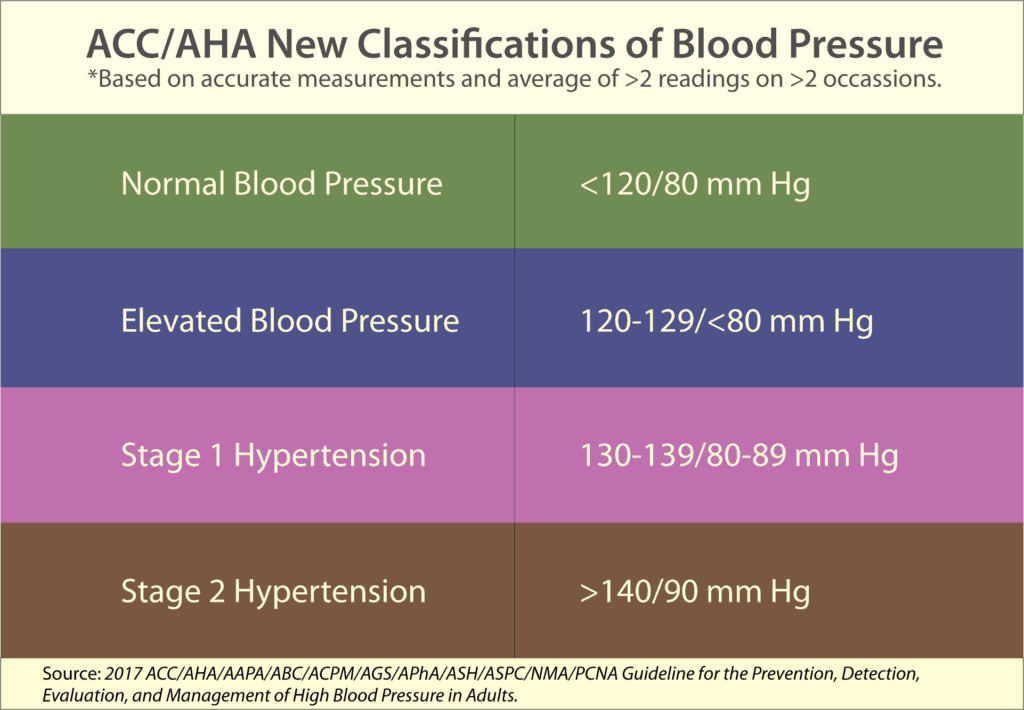
- Lowering blood pressure. When left untreated high blood pressure can lead to stroke and heart disease. In 2021, a systematic review and meta-analysis that looked at six studies concluded that Mindfulness Based Stress Reduction (MBSR) contributed to a reduction in both systolic and diastolic blood pressure in hypertensive and prehypertensive participants.
- Releasing feelings of stress and tension. Meditating quietly even for just a few minutes a day can restore feelings of calm and peacefulness. In a 2021 study on nursing students, researchers reported a significant reduction of anxiety and stress after engaging in mind-body techniques such as meditation over a period of time.
- Improving sleep. Evidence shows that mindfulness meditation can be successfully used for the treatment of insomnia.
- Improving the response to emotional stimuli. After an 8-week period, the researchers in this 2016 study reported “…MBSR led to changes in the amygdala consistent with improved emotion regulation.”
- Boosting the immune system. After an 8-week period, the researchers in this study in Psychosomatic Medicine reported “demonstrable effects on brain and immune function.”
- Reducing inflammation. Inflammation plays a major role in heart disease. Chronic inflammation is involved in all stages of atherosclerosis, the process that leads to cholesterol-clogged arteries. Practicing a mind-body therapy such as meditation, in adjunct with dietary and exercise programs, can help reduce underlying inflammatory processes.
The bottom line: Meditation is a practice that you can do anywhere at any time, alone in the privacy of your own home, or in the company of others. As with many things in life, getting started is the hardest step. Private consultations with a trained practitioner can be a wonderful way for you to take that first step or to enhance an existing practice.
Below you’ll find some additional studies that demonstrate the positive effects of meditation, as well as yoga (which incorporates many of the wonderful elements of meditation), on cardiovascular health.
- Association Between Mind-Body Practice and Cardiometabolic Risk Factors: The Rotterdam Study.
- Meditation and coronary heart disease: a review of the current clinical evidence.
- Systematic Review of Yoga Interventions to Promote Cardiovascular Health in Older Adults.
- Yoga as an Alternative and Complementary Therapy for Cardiovascular Disease: A Systematic Review.
In the battle against stress and even heart disease, there is a lot you can do! By being proactive now, you can bring about changes that can make a significant difference in how you feel, both physically and emotionally, in the very near future.
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
This article first appeared in Dr. Kaplan’s column on MindBodyGreen.com. Reviewed and updated April, 2024.