4 Ways to Practice Gratitude During the Holidays
Thanksgiving is a wonderful holiday tradition that’s been celebrated in the US and Canada since the mid-1800s. At the heart of the Thanksgiving celebration is the universal message of gratitude.
Gratitude is the expression of being thankful. It’s about having an attitude of appreciation, allowing yourself to feel awe, not taking things for granted, and seeing the potential upside of life’s challenges. But did you know that practicing gratitude can have profound benefits to our mental, emotional and physical well-being?
Let’s take a closer look at how practicing gratitude can contribute to our overall well-being and some effective ways to incorporate this practice into our daily lives.
The Link Between Gratitude and Well-Being
Practicing gratitude can benefit the mind, body, and spirit in a number of ways. It can lower stress levels, improve sleep, strengthen relationships with friends and family, and even increase our emotional resilience. Medical research has confirmed this direct correlation between gratitude and well-being:
- A 2022 study published in Frontiers of Psychology found that women with elevated depressive symptoms who routinely practiced gratitude were more accepting of their condition than those who did not. Similarly, a 2012 study published in Personality and Individual Differences found that people who regularly expressed gratitude reported feeling healthier than their counterparts; a correlation that was mediated by psychological health and an attitude to seek help for health concerns.
- A 2018 abstract, printed in the journal Psychology, Health & Medicine, found that dispositional gratitude (i.e. the character trait of noticing and appreciating the positive in life and being thankful for those positive aspects of life) correlated with lower levels of stress and loneliness.
- Practicing gratitude can improve sleep quality by promoting more positive emotions and lessening the effects of anxiety and rumination.
- In a 2013 study, Dr. Robert Emmons, a leading authority on gratitude, noted that: “Gratitude is a key, underappreciated quality in the clinical practice of psychology, its relevance deriving from its strong, unique, and causal relationship with well-being, as well as its dynamic healing influence on the therapist-patient relationship.”
- Acts of kindness (public expressions of gratitude) can be linked to an increase in life satisfaction, according to a study published in The Journal of Social Psychology.
- Researchers who looked at the role of gratitude in asymptomatic heart failure patients found that “patients expressing more gratitude also had lower levels of inflammatory biomarkers,” as well as better sleep and mood, and less fatigue.
Questions? Give Us a Call!
How to Cultivate Gratitude
Practicing gratitude is a conscious choice we make to affect positive change in our lives. There are a number of ways to practice gratitude, such as:
Appreciate nature
Beauty is everywhere. Taking a moment to stop and experience the beauty in nature can provide you with a greater sense of well-being that can stay with you throughout the day. As you walk or observe, mentally list the things that bring you joy, peace, or fulfillment.
Keep a gratitude diary
Write down 5 or 6 things daily for which you are grateful. Recognizing what you are grateful for will help keep you focused on what you have rather than what you have not and creates a record of appreciation to look back on when you need a mood boost.
Meditate
A daily meditation practice, for even just a few minutes a day, helps reset your body’s autonomic stress response, which can help to improve sleep, reduce pain, enhance mood, and foster a better sense of well-being.
Say “Thank you.”
Taking the time to thank others, whether through a note, a text message, or a face-to-face conversation, not only uplifts their spirits but also helps reinforce your own sense of appreciation. This practice nurtures social bonds and fosters a greater sense of connection and well-being.
As we prepare for another Thanksgiving holiday in the US, it’s my wish that gratitude and all its benefits be present in your life and the lives of those you care about. And I wish you and yours a very happy and healthy Thanksgiving.
– Dr. Gary
We are here for you, and we want to help.
Our goal is to return you to optimal health as soon as possible. To schedule an appointment please call: 703-532-4892 x2
Updated: November 2024
References
Tomczyk J, Nezlek JB, Krejtz I. Gratitude Can Help Women At-Risk for Depression Accept Their Depressive Symptoms, Which Leads to Improved Mental Health. Front Psychol. 2022 Apr 7;13:878819. doi: 10.3389/fpsyg.2022.878819. PMID: 35465539; PMCID: PMC9022718.
Hill PL, Allemand M, Roberts BW. Examining the Pathways between Gratitude and Self-Rated Physical Health across Adulthood. Pers Individ Dif. 2013 Jan;54(1):92-96. doi: 10.1016/j.paid.2012.08.011. PMID: 23139438; PMCID: PMC3489271.
O’Connell BH, Killeen-Byrt M. Psychosocial health mediates the gratitude-physical health link. Psychol Health Med. 2018 Oct;23(9):1145-1150. doi: 10.1080/13548506.2018.1469782. Epub 2018 Apr 29. PMID: 29707980.
Emmons RA, Stern R. Gratitude as a psychotherapeutic intervention. J Clin Psychol. 2013 Aug;69(8):846-55. doi: 10.1002/jclp.22020. Epub 2013 Jun 17. PMID: 23775470.
Jia Wei Zhang, Ryan T. Howell, Ravi Iyer, Engagement with natural beauty moderates the positive relation between connectedness with nature and psychological well-being, Journal of Environmental Psychology, Volume 38, 2014, Pages 55-63, ISSN 0272-4944, https://doi.org/10.1016/j.jenvp.2013.12.013.
Rowland L, Curry OS. A range of kindness activities boost happiness. J Soc Psychol. 2019;159(3):340-343. doi: 10.1080/00224545.2018.1469461. Epub 2018 May 15. PMID: 29702043.
Mills PJ, Redwine L, Wilson K, Pung MA, Chinh K, Greenberg BH, Lunde O, Maisel A, Raisinghani A, Wood A, Chopra D. The Role of Gratitude in Spiritual Well-being in Asymptomatic Heart Failure Patients. Spiritual Clin Pract (Wash D C ). 2015 Mar;2(1):5-17. doi: 10.1037/scp0000050. PMID: 26203459; PMCID: PMC4507265.




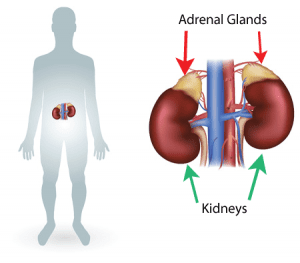 Adrenal Hold
Adrenal Hold




